Low-Dose CT Protocol Optimization Plan
Achieving Ultra-Low-Dose (DLP < 160 mGy*cm) in Hybrid & Standalone CT
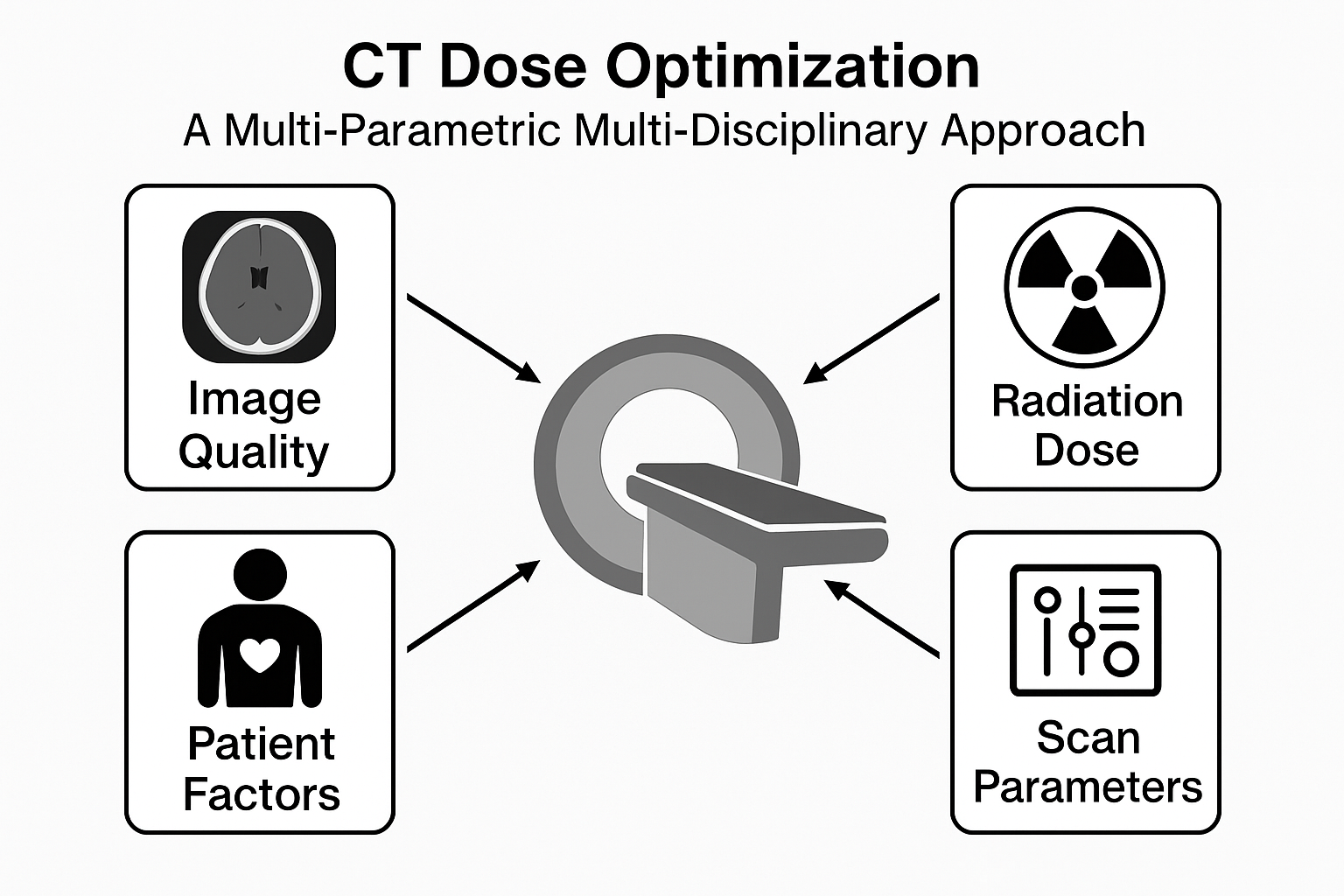
Project Objective & Scope
This plan outlines the primary objective and scope for a comprehensive study to optimize CT protocols. The central goal is to achieve low-dose (LD) or ultra-low-dose (ULD) scans across a variety of scanners, defined by a target Dose Length Product (DLP) of less than 160 mGy*cm for a whole body scan. This specific threshold is often a Diagnostic Reference Level (DRL) for chest/abdominal screening or an accepted limit for hybrid CT attenuation correction, and is critical for minimizing patient radiation exposure, especially in repeat-scan scenarios like CT screening, PET/CT and SPECT/CT attenuation correction (AC) and organ delineation for Radionuclide therapy dosimetry.
Targeted Scanners
- Standalone Diagnostic CT
- PET/CT Hybrid Scanners
- SPECT/CT Hybrid Scanners
Manufacturer Focus
- Siemens Healthineers
- GE Healthcare
- Philips Healthcare
- Fujifilm Healthcare
- Canon Medical Systems
Key Consideration: No Shielding
This plan explicitly excludes the use of bismuth shielding for radiosensitive tissues. Research indicates this practice is often ineffective and may increase dose due to beam-hardening artifacts and back-scatter, and interfere with automatic exposure control (AEC) systems.
Core Dose Reduction Techniques
This section details the core parameters that will be manipulated to achieve the dose reduction target. Each technique presents a trade-off between dose and image quality, which will be managed by the advanced reconstruction algorithms. Click each card to learn more about the rationale.
Low Kilovoltage (kV) ▼
Rationale: Lowering kV (e.g., 100 kV or 80 kV) dramatically reduces dose (dose ~ kV²). It also increases the photoelectric effect, boosting contrast for iodinated media.
Challenge: Increases image noise and potential for photon starvation artifacts in larger patients.
Mitigation: Compensated by advanced iterative or DL reconstruction to manage noise.
Low Tube Current (mA) ▼
Rationale: Dose is directly proportional to the mAs (mA * rotation time). Using Automatic Exposure Control (AEC) with a very low "noise index" or quality reference mAs is a primary method for dose reduction.
Challenge: Directly increases quantum noise, which can obscure low-contrast structures.
Mitigation: This is the primary challenge that DL reconstruction is designed to overcome.
High Pitch ▼
Rationale: A higher pitch (table travel per rotation / collimation) reduces scan time and radiation exposure for a given scan length, as the x-ray beam spends less time on each voxel.
Challenge: Can introduce spiral artifacts and broaden the slice sensitivity profile, slightly reducing z-axis resolution.
Mitigation: Modern multi-slice scanners (64+) and their reconstruction algorithms handle high-pitch (up to 1.5-2.0) scans effectively.
Reduced Scan Area ▼
Rationale: Particularly for PET/CT and SPECT/CT, the CT scan is only needed for attenuation correction (AC) and anatomical localization. The scan length can often be limited to the PET/SPECT acquisition field-of-view, avoiding a full diagnostic-length scan.
Challenge: Requires careful protocoling to ensure the AC map (μ-map) covers the entire relevant emission volume to prevent truncation artifacts in the final PET/SPECT image.
Reconstruction Technologies: IR vs. Deep Learning (DLIR)
The ultimate enabler of ultra-low-dose CT is the reconstruction algorithm, which manages the massive increase in image noise resulting from lower mA and kV. Our plan will focus on optimizing two generations of reconstruction technology: Iterative Reconstruction (IR) and the latest Deep Learning (DLIR) solutions.
Iterative Reconstruction (IR)
IR algorithms (like ASiR, SAFIRE, iDose4) use a statistical or model-based approach to correct for noise and artifacts over multiple cycles. They are a proven tool for reducing dose by 30-60%, but often introduce a distinct "blotchy" or plastic-like noise texture that can obscure fine details and affect segmentation.
Deep Learning Reconstruction (DLIR)
DLIR (like TrueFidelity, AiCE, Precise Image) uses a neural network trained on thousands of high-quality, full-dose scans. It performs image transformation to mimic the texture of a full-dose FBP (Filtered Back Projection) image while suppressing noise from ultra-low-dose acquisition. DLIR can achieve dose reductions beyond 80%.
Figure 2: Deep Learning CT Reconstruction Flowchart
1. Low-Dose Acquisition
Raw Data (Sinogram) or Initial FBP Image from Ultra-Low mAs/kV Scan
2. Deep Learning Network (Trained Model)
- Input image fed into the **Convolutional Neural Network (CNN)**.
- Network applies learned filters to optimally denoise and restore image texture.
3. High-Quality Diagnostic Output
Image with **Full-Dose FBP Texture** but with ultra-low noise levels (Denoised, High-Resolution).
The DLIR model is pre-trained using paired low-dose and full-dose images to learn the transformation that optimally removes noise while preserving anatomical texture and resolution.
Specialized Protocols: Pediatric and Pregnancy Focus
A critical component of this research is lowering dose to children who are more radiosensitive. Protocols designed for children must be weight and/or age based, and adhere to strict DLP limits based on pediatric DRL (Diagnostic reference Levels) which should be monitored routinely using a DMS (Dose Management System) while maintaining diagnostic image quality for the specific task and indication.
Another group of special focus are pregnant or potentially pregnant woman, who require protocols designed to limit dose to uterus. In some cases, the retrospective and prospective dose to the embryo is estimated, and risk assessments are performed and discussed in MDT (Multi Disciplinary Teams) to assess along with the patient the next steps.
For the purpose of prospective dose estimates many free and commercial software exist to find effective dose based on Monte Carlo derived dose coefficients for specific phantoms and protocol settings such as:
- ImPACT CT (St George’s NHS, UK)
- MIRDct (MIRDsoft, USA)
- NCICT / NCIDose (NCI USA)
- VirtualDose™ CT (Virtual Phantoms Inc. USA)
- CT-Expo (Germany)
Note: Some of these software are no longer in active development so the scanner list available may be outdated.
Vendor-Specific Tools
Each CT manufacturer provides proprietary tools for dose reduction and image quality enhancement. This section allows exploration of the key technologies from each vendor that will be evaluated in this study. Click a vendor name to see its relevant reconstruction and artifact reduction tools.
Implementation and QA Checklist
To validate the low-dose protocols, a rigorous quantitative and qualitative assessment is required. This assessment must confirm that the resulting images are sufficient for their intended task, particularly for attenuation correction and organ segmentation in therapy dosimetry.
- Protocol Creation: For each modality (CT only, PET/CT, SPECT/CT) and patient type (adult, child), create dedicated protocols. Set scan range, kVp, pitch, reference mA (or noise index) according to the above guidelines. Document the expected CTDI_vol and DLP.
- Dose Monitoring: After scanning CTDI phantom, verify the actual DLP is below specified threshold such as 160 mGy*cm. Use the built-in dose report. Track these values for all patients over time with a Dose Management and Monitoring system such as: DOSE (Qaelum), DoseM (Infinitt), DoseMonitor (PACS Health), DoseTrack (Sectra), DoseWatch (GE), DoseWise (Philips), OpenRem (free), teamplay (Siemens).
- Phantom Testing: Scan an ACR phantom at each low-dose protocol. Measure high-contrast resolution (should meet ACR pass limits) and low-contrast detectability. Compute NPS and MTF and compare against a baseline (full-dose) scan. Adjust IR levels until image quality metrics are acceptable.
- Clinical Review: Have radiologists/nuclear physicians review images from pilot scans (especially pediatric and PET/CT) to ensure lesions are still detectable and structures can be defined as needed. Use their feedback to tweak IR strength or slightly raise mA if needed.
- Education and Safety: Train technologists in selecting the correct protocol (especially pediatric ones). Remind staff of the DLP goal as a key criterion. If new software or hardware is installed or updated, re-validate the low-dose protocols.
Hypothesized Dose vs. Image Quality
Figure 1: Hypothesized relationship between dose and image quality for different reconstruction levels. The goal is to move towards the top-left.
Image quality will be objectively assessed using phantoms (e.g., Catphan) to measure key performance indicators:
- Modulation Transfer Function (MTF): To quantify spatial resolution. We must ensure that low-dose protocols do not unacceptably blur fine details, which is critical for defining organ edges.
- Noise Power Spectrum (NPS): To characterize the magnitude and texture of image noise. This is more descriptive than simple standard deviation, as DL algorithms can alter the noise texture (e.g., make it "blotchy"), which may affect segmentation algorithms differently than simple quantum noise.
- Contrast-to-Noise Ratio (CNR): To ensure that low-contrast objects remain distinguishable.
- HU Accuracy: To confirm that CT numbers remain stable, which is non-negotiable for accurate attenuation correction in PET/SPECT.
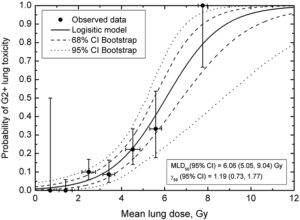
The ultimate test is fitness-for-purpose. We will assess the impact of ULD images on two key clinical tasks:
- Attenuation Correction (AC): We will compare PET and SPECT reconstructions using ULD-CT μ-maps versus standard-dose μ-maps. We will quantify differences in tracer uptake values (SUVs) in key regions to ensure no clinically significant bias is introduced.
- Radionuclide Therapy Dosimetry: This is highly sensitive to image quality. We will evaluate the ability to segment organs (e.g., kidneys, liver, spleen) on ULD-CT images, both manually and with common auto-segmentation tools. Degradation in edge definition (measured by MTF) or changes in noise texture (measured by NPS) could lead to inaccurate volume delineation and, therefore, incorrect absorbed dose calculations.