
1. What is the main advantage of Fluoroscopy?
Currently, the most reliable and widely used imaging modalities that can provide real-time changes in vasculature with up to 30 frames per second are unfortunately ionising and include fluoroscopy and angiography.
They are essential imaging modalities in interventional procedures, particularly in cardiac and neurosurgery. These procedures typically require high temporal resolution to accurately visualize fast-moving structures such as the beating heart or cerebral blood flow. However, most acceptance and commissioning tests often neglect temporal testing, focusing primarily on dose rates for common protocols and static image quality metrics like spatial resolution and contrast measurements. This oversight can lead to clinicians missing important aspects, due to motion blur, ghosting artifacts, frame averaging, and misregistration errors, impacting surgical precision and patient safety.
On the other hand, high frames per second, which is also high dose rate, is not necessary in all procedures and situations, but without testing the exact relationship between frames and dose, we can’t optimize procedures. In other words, just because a fluoroscopy system is producing X pulses per second, that does not mean it is also capturing X different frames per second. The X-ray system is independent of the imaging system, and as such, should be independently evaluated.
This article highlights the current gaps in fluoroscopy testing, impact of temporal tests on clinical procedures (or lack thereof), reasons why comprehensive tests should be included in acceptance of new protocols/systems, and the tools and phantoms available to improve system performance.
In the end, the potential benefits of integrating temporal resolution assessments should be evident, ensuring real-time imaging is optimized for critical interventions.
The article will not deal with ultrasound, which can also provide real time imaging of the heart, but lacks penetration ability, and has a much smaller Field of View (FoV), and does not provide the same clinical value as fluoroscopy.
2. Current Situation: Gaps in Temporal Resolution Testing
In most medical physics acceptance testing, tests focus on static image quality metrics such as contrast-to-noise ratio (CNR), spatial resolution, and detector uniformity. While these are critical for fluoroscopy and angiography, they do not account for motion-related artifacts that can degrade real-time imaging.
Common issues due to the lack of temporal resolution testing include:
- Motion blur in dynamic imaging, reducing vessel and implanted device clarity.
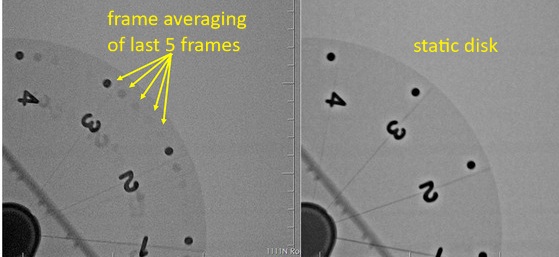
- Frame lag and ghosting artifacts, making it harder to track stents, guidewires, and catheters.
- Misregistration in Digital Subtraction Angiography (DSA), leading to inaccurate vessel visualization.
- Increased radiation dose, as operators compensate for poor imaging by increasing exposure time.
Despite these issues, most Quality Assurance programs do not include temporal tests, either at acceptance or at routine intervals, largely due to:
- Lack of standardized temporal testing protocols compared to spatial resolution tests.
- Complexity of motion simulation, requiring specialized equipment, which may be expensive and hard to obtain.
- Reliance on manufacturers’ built-in compensation algorithms, like digital frame averaging, which do not always perform optimally in clinical settings, and often operate like black boxes.
- Lack of regulations and guidelines necessitating the need for temporal testing, which leaves specific and specialized temporal tests at the discretion of the medical physicist.
3. Clinical Impact: Brain and Cardiac Surgery Risks
Lack of proper temporal resolution assessment can lead to significant risks in high-precision interventional procedures, especially in the heart and brain, where fast-moving structures demand real-time accuracy.
3.1 Cardiac Interventions
Coronary angioplasty and stent placement require real-time imaging to track guidewires and balloon catheters.
Poor temporal resolution can cause motion blur, making it difficult to determine precise device positioning.
Pulsatile coronary artery motion may appear smeared, increasing the risk of misplacing a stent.
3.2 Neurosurgical and Stroke Procedures
DSA is critical for stroke thrombectomy, aneurysm coiling, and AVM embolization.
Frame lag and motion artifacts can lead to misregistration errors, misguiding clot retrieval devices.
In carotid artery stenting, low temporal resolution can make it harder to detect flow abnormalities post-deployment.
Delayed image updates or motion-related blurring can cause surgeons to misinterpret vessel dynamics, leading to procedural complications or increased intervention time.
4. Why Temporal Resolution Tests Should Be Added during acceptance testing of Fluoroscopy
To ensure imaging systems function optimally during dynamic procedures, medical physicists should incorporate temporal testing into Quality Assurance protocols either at acceptance or when new protocols are introduced in clinical practice.
Key reasons to implement temporal tests:
- Confirms real-time visualization, ensuring accurate device tracking in fast-moving structures.
- Pinpoints under what conditions motion artifacts may obscure critical anatomical details, and how to minimize them.
- Prevents unnecessary radiation exposure by avoiding prolonged fluoroscopy time. Therefore, ionising radiation to both patients and staff in the operating theatre can be effectively reduced. In Europe and the UK, this will make it easier to remain as close as possible to established Diagnostic Reference Levels for specific procedures.
- Ensures system compliance with manufacturer and/or national specifications for frame rate and pulsed fluoroscopy response time (see NEMA in references).
- Optimizes DSA image subtraction accuracy, improving diagnostic and procedural confidence.
By integrating motion phantoms, pulsed frame rate tests, and automated motion analysis software, medical physicists can quantify and correct temporal resolution deficiencies.
5. Tools and Phantoms for Temporal Resolution Testing
To evaluate and optimize fluoroscopic and angiographic systems for motion performance, the following tools are recommended:
MOTUS Motion Platform (Leeds Test Objects, UK)
Programmable movement in the Z-axis (0–7.5 cm/s) with optional Y-axis motion.
Enables testing of motion artifacts in real-time imaging.
QUART DSA Phantom (QUART GmbH, Germany)
Assesses DSA misregistration and temporal resolution in vascular imaging.
Model L-629 Rotating Spoke Test Tool (Ludlum Measurements, Inc., TX, USA)
The L-629 Rotating Spoke Test Pattern consists of a circular 5.5 inch diameter acrylic disk with steel 12 wires arranged on its surface in 30 degree intervals. Lead numbers (1-6) appear on each half of the disk near the perimeter. The disk is mounted on a synchronous motor with a speed of 30 RPM to simulate movement of wires.
6. Impact of Implementing Temporal Resolution Tests
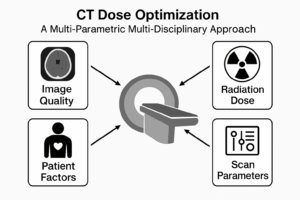
Based on multi-disciplinary meetings, with input from the medical physicist, interventional radiologist, and radiographer, the appropriate settings of pulse width and frame averaging can be selected on most fluoroscopy and angiography systems, from most major manufacturers.
When motion-related tests are integrated into imaging system evaluations during acceptance or commissioning, the benefits include:
✅ Enhanced Surgical Precision – Surgeons can rely on sharper, real-time imaging for accurate device placement.
✅ Reduced Motion Blur & Ghosting Artifacts – Ensures clear visualization of fast-moving vessels and devices, by using optimized protocols.
For example, we can reduce motion blurring by reducing pulse width, on most old fluoroscopy systems.
In addition we can reduce ghosting by reducing frame averaging. This is possible on most new angiography systems by modifying parameters like “Temporal Filtering”, “Noise Reduction”, or “Recursive Filtering” depending on vendor.
✅ Lower Radiation Exposure – Operators won’t need to increase exposure time to compensate for poor imaging.
✅ Optimized System Performance – Testing ensures angiography and fluoroscopy systems operate within optimal parameters.
✅ Fewer Procedural Errors – Better temporal resolution, leads to improved patient outcomes, reduced complications, recovery times, and associated healthcare costs.
By improving dynamic imaging quality, hospitals and medical centers can boost surgical success in high-risk procedures.
7. Conclusion
Current testing protocols often overlook temporal resolution testing, despite its critical role in fluoroscopy and angiography. Cardiac and neurosurgical interventions demand real-time, high-frame-rate imaging to ensure precision and safety. By integrating motion phantoms, pulsed frame rate tools, and automated analysis software, hospitals can improve real-time imaging quality, reduce motion artifacts, and optimize interventional procedures.
Medical physicists should advocate for routine temporal resolution assessments, ensuring fluoroscopic systems meet the demands of high-risk cardiac and neuro interventions. Implementing these tests will lead to safer, more effective procedures, ultimately improving patient outcomes.
References
- AAPM Report No. 125. Quality Control in Fluoroscopy. American Association of Physicists in Medicine.
- AAPM Task Group 142. Quality Assurance of Fluoroscopic and Angiographic Systems. American Association of Physicists in Medicine.
- Anthony, G., Liang, Y., & Zhao, X. (2022). Performance evaluation of two interventional fluoroscope suites for cardiovascular imaging. Journal of Applied Clinical Medical Physics, 23(10), e13741.
- Hirsch, J. A., et al. (2015). Quality Improvement Guidelines for Digital Subtraction Angiography. Journal of NeuroInterventional Surgery.
- ICRP Publication 135. Diagnostic Reference Levels in Medical Imaging. International Commission on Radiological Protection.
- Klein, L. W., et al. (2010). The Importance of Temporal Resolution in Cardiac Imaging. Journal of the American College of Cardiology.
- Leeds Test Objects. MOTUS Motion Phantom & DynamIQ Software. [Online] Available at: https://www.leedstestobjects.com
- QUART GmbH. DSA and Temporal Resolution Phantoms. [Online] Available at: https://www.quart.de
- Smith, W. S., et al. (2015). Mechanical Thrombectomy for Acute Ischemic Stroke. Stroke.
- Zhou, W., & Lin, P. J. (2018). Advances in Fluoroscopic Imaging Technology. Medical Physics International.
- NEMA Standards Publication NU 1-2018. Performance Measurements of Angiographic and Fluoroscopic Systems. National Electrical Manufacturers Association.



Interesting read, thank you. Ghosting is an annoying artefact I find.