Current status of MRI QA
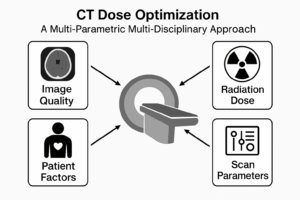
Nowadays modern Magnetic Resonance Imaging (MRI) scanners have a plethora of programs, pulses sequences, transmitting / receiving coils, and are utilised extensively on symptomatic pregnant women, children and young adults, because they are safer than Computed Tomography (CT), and even asymptomatic patients as a screening tool.
Most regulatory authorities do not enforce MRI Quality Assurance (QA) because it is not an ionising modality. When some tests are performed to check image quality, as part of acceptance or routine quality assurance, most guidelines are satisfied with very basic QA using manufacturer recommendations and/or the outdated ACR MRI phantom, designed 40 years ago, for the MRIs of that era.
The static ACR MRI phantom is typically scanned using a simple Spin Echo, T1 or T2 weighted pulse sequence, and does not allow for testing complicated pulse sequences.
Curious about better ways to test MRI systems? Below is a list of some advanced MRI QA tests that go beyond the standard ACR phantom tests, ensuring higher precision, better functional imaging accuracy, and tighter tolerances which show the superiority of newer/more advanced MRI systems, in diagnosis and disease progression.
1. Functional MRI (fMRI) Stability and Drift Test
Why? fMRI measures small changes in blood oxygenation (Blood Oxygen Level Dependent signal or BOLD), but current QA does not track long-term signal drift or scanner stability over time.
How?
- Use an fMRI stability phantom (e.g., agar-based or oil-water mixtures) and run a resting-state fMRI sequence for at least 10–20 minutes.
- Measure temporal SNR (tSNR) and check for slow signal drifts (>1% over 10 min would be unacceptable).
- Assess spatial variability across different regions to ensure uniformity.
2. Diffusion Tensor Imaging (DTI) Gradient Linearity and Eddy Current Test
Why? DTI is sensitive to gradient non-linearity and eddy currents, which distort tensor calculations and fiber tracking, but standard QA does not evaluate these effects.
How?
- Scan a diffusion phantom containing capillary structures or structured grids in multiple gradient orientations.
- Quantify mean diffusivity (MD) and fractional anisotropy (FA) across different b-values and ensure deviations are <5% from baseline.
- Assess gradient non-linearity by checking for systematic shifts in calculated diffusion tensors.
3. Magnetic Resonance Spectroscopy (MRS) Linewidth and Metabolite Drift Test
Why? MRS requires high spectral resolution, and scanner instability can degrade metabolite peak accuracy, but this is rarely tested in standard QA.
How?
- Use an MRS phantom with known metabolite concentrations (e.g., NAA, lactate, choline, creatine).
- Measure linewidth (FWHM) and peak separation for key metabolites.
- Compare current measurements to baseline, ensuring drift remains <3%.
- Evaluate SNR degradation over time, rejecting systems where SNR drops >10% over 1 year.
4. Tighter SNR Tolerance to Promote Newer Systems
Why? Most MRI scanners pass ACR SNR thresholds easily, but older systems may have significant hidden degradation in real-world scans.
How?
- Require minimum SNR levels for 3T scanners (>300) and for 1.5T (>150) in uniform phantom scans.
- Use parallel imaging (GRAPPA/SENSE) tests to check whether SNR losses exceed acceptable levels (e.g., >20% drop at R=3 acceleration).
- Test high-bandwidth sequences, as older systems often show excessive noise at BW >500 Hz/pixel.
5. Parallel Imaging & Multi-Band Factor Stability Test
Why? Many modern MRI studies rely on GRAPPA, SENSE, and multi-band EPI, but QA does not check if acceleration is degrading image quality.
How?
- Scan a uniform phantom using parallel imaging (GRAPPA R=2 to R=4) and compare noise amplification (g-factor).
- Test multi-band EPI sequences and check for slice leakage artifacts.
- Ensure g-factor scaling remains <1.5x the expected value for a given acceleration.
6. Ultra-High-Resolution Spatial Fidelity Check
Why? Many MRI exams now require sub-millimeter resolution (e.g., 7T imaging, high-res fMRI for the brain), but scanner QA does not verify geometric precision at this scale.
How?
- Use a grid phantom with sub-mm structures (e.g., 0.5mm resolution) and scan with a 0.4mm isotropic resolution sequence.
- Check for geometric distortions larger than 0.2mm over 10cm, as older systems often fail at sub-mm precision.
7. Dynamic B0 Field Stability & Susceptibility Correction Test
Why? B0 drift over time degrades spectroscopy, EPI, and fMRI, but current QA does not check field stability dynamically.
How?
- Use a FID navigator sequence to track B0 shifts over 10–30 min scans.
- Ensure drift is <0.1 ppm/min over 30 minutes, failing scanners that exceed this.
- Test EPI-based distortion correction and require that warping is reduced by >80% post-correction.
8. RF Transmit and Receive Homogeneity Mapping
Why? Inhomogeneous RF fields (B1+) cause signal dropouts and incorrect quantification in quantitative MRI (qMRI), but standard QA does not assess this.
How?
- Use B1 mapping sequences (AFI, DREAM, or actual flip angle mapping) to check RF homogeneity across the field of view.
- Require that B1+ deviations remain <10% across the brain, as larger deviations lead to poor quantitative accuracy.
9. Extreme Case Fat Suppression & Chemical Shift Test
Why? Poor fat suppression affects MRCP, breast MRI, and musculoskeletal imaging, but standard QA does not push fat saturation to failure points.
How?
- Scan a phantom with strong B0 inhomogeneity and lipid components using different fat suppression techniques (CHESS, Dixon, STIR, SPIR).
- Identify regions where suppression fails (>20% residual fat signal), indicating poor shimming or RF non-uniformity.
10. Artifact Challenge Protocol
Why? Standard QA does not evaluate real-world artifacts like RF noise, vibration, and aliasing.
How?
- Run sequences in an intentional interference environment (e.g., near an RF source or with physical vibration, as commonly found in a hospital environment).
- Score the severity of ghosting, Nyquist ghosts, and RF interference.
- Require artifact levels to remain within predefined thresholds, failing scanners that exceed acceptable noise levels.
Summary of Uncommon MRI QA Tests
Test Name | Purpose | How It Challenges Older Scanners |
fMRI Stability Test | Ensures no BOLD signal drift | Exposes long-term scanner drift |
DTI Gradient Linearity Test | Checks tensor integrity | Identifies non-linear gradient errors |
MRS Linewidth & Metabolite Test | Assesses spectral resolution | Flags scanners with poor spectral quality |
Tighter SNR Tolerances | Disqualifies noisy systems | Older scanners struggle to meet higher SNR |
Parallel Imaging QA | Evaluates GRAPPA/SENSE efficiency | Older systems show higher noise amplification |
Ultra-High-Resolution Fidelity | Tests sub-mm accuracy | Older scanners fail geometric precision tests |
B0 Stability Test | Ensures field uniformity | Identifies frequency drift issues |
B1 Homogeneity Mapping | Ensures uniform RF transmission | Exposes transmit/receive coil problems |
Fat Suppression Stress Test | Pushes suppression techniques to limits | Finds failures in fat suppression methods |
Artifact Challenge Protocol | Tests scanner robustness | Identifies real-world artifact susceptibility |
Clinical Impact of incomplete Quality Assurance
The clinical impact of not performing the advanced MRI QA tests outlined in the article can be significant, affecting diagnostic accuracy, patient safety, and healthcare costs. Below are the key consequences:
1. Reduced Diagnostic Accuracy
- fMRI Stability Issues: If fMRI scanners are not tested for long-term signal drift, small changes in brain activity may be misinterpreted, leading to misdiagnoses in neurological disorders like stroke, epilepsy, or psychiatric conditions.
- DTI Gradient Non-linearity: Without gradient linearity testing, fiber tracking in white matter diseases (e.g., multiple sclerosis, traumatic brain injury) may be distorted, leading to incorrect conclusions.
- MRS Spectral Degradation: If magnetic resonance spectroscopy (MRS) is not checked for metabolite drift, biochemical markers for diseases like brain tumors, Alzheimer’s, and metabolic disorders may be miscalculated, affecting treatment plans.
2. False Negatives & Missed Diagnoses
- Poor SNR Tolerance: Older MRI systems with hidden signal degradation may fail to detect small lesions in cancer screening (e.g., breast MRI, prostate MRI).
- Inadequate Fat Suppression: In musculoskeletal and breast MRI, improper fat suppression can obscure pathology, leading to missed tumors or inflammatory conditions.
- Ultra-High-Resolution Failures: If spatial fidelity is not validated, sub-millimeter lesions in the brain, spine, or joints may be missed, delaying treatment.
3. Increased Patient Risks & Unnecessary Procedures
- Artifact Issues: Without artifact testing, ghosting, aliasing, and RF noise may mimic pathology, leading to false positives and unnecessary follow-ups, biopsies, or even surgeries.
- Inaccurate B0/B1 Mapping: Poor B0 stability affects fMRI and diffusion imaging, while B1 inhomogeneity causes errors in quantitative MRI (qMRI), impacting treatment planning for diseases like cancer or liver fibrosis.
- Eddy Currents in DTI: If eddy currents distort diffusion imaging, patients with suspected stroke or neurodegenerative diseases may receive incorrect diagnoses.
4. Wasted Resources & Increased Healthcare Costs
- Repeat Scans: Poor QA leads to non-diagnostic scans, forcing re-scanning, increasing hospital costs, scanner downtime, and patient inconvenience.
- Legal & Regulatory Issues: If an MRI scanner produces inconsistent results, hospitals may face legal liability or regulatory penalties.
- Competitive Disadvantage: Institutions failing to meet higher QA standards may lose credibility, impacting research and patient trust.
5. Poor Treatment Monitoring
- fMRI & BOLD Signal Drift: Inconsistent fMRI signals affect brain function mapping, impacting surgical planning for epilepsy, tumors, or deep brain stimulation (DBS).
- DTI Variability: If diffusion imaging lacks consistency, monitoring disease progression in multiple sclerosis (MS) or ALS becomes unreliable.
- SNR Drop in Follow-ups: Without strict SNR testing, follow-up MRIs may show artificial changes in tumors or lesions, leading to unnecessary changes in treatment.
Conclusion: The Need for Stricter MRI QA
By not conducting these uncommon but crucial MRI QA tests, false diagnoses, increased healthcare costs, and patient harm become real risks.
Call to Action
All of the tests described here require two sides of the same coin:
- Experienced personnel like medical physicists, radiographers, technologists, and radiologists with enough time and the right tools and phantoms to perform, analyze and interpret the results of the above tests.
- A requirement by regulators, policy makers, and healthcare authorities that MRI scanners pass all relevant tests, depending on clinical use. Strict enforcement can be achieved with penalties when the tests are not performed or results not provided in time.
One could say that 1 and 2 above are like the chicken and egg problem, nobody knows which comes first, but the process has to start somewhere, and it starts with you.
Whether you work in healthcare, a regulatory authority, or you are an MRI patient, seek higher standards in MRI image quality, and routinely ask how the lack of comprehensive MRI QA is impacting you.